/ A NEGLECTED DISEASE
Noma is a neglected disease that affects people living in poverty. It’s an infectious but non-contagious bacterial disease that starts as an inflammation of the gums, similar to a small mouth ulcer. The infection destroys the bone and tissue very quickly, affecting the jaw, lips, cheeks, nose or eyes, depending on where the infection started.
It takes just days for noma to leave survivors with severe facial disfigurements that make it hard to eat, speak, see or breathe. On top of that, survivors must deal with the social stigma caused by the horrific damage done to the face.
Noma mostly affects children under seven years old who are living in poverty. Poverty and poor health are the main factors behind the infection that leads to noma. Children with malnutrition, bad oral hygiene and diseases such as measles or malaria are particularly susceptible to noma.
People who survive noma have only one choice if they want a better life: they must undergo extensive reconstructive surgery.
How many people die of Noma?
of people affected by noma die in the first two weeks if they don’t receive treatment with antibiotics in time. That’s why early detection and awareness raising campaigns are so important for a disease that affects an estimated 140,000 children every year. *

*These numbers are an estimate that the World Health Organization (WHO) made in 1994. The fact this data has not been updated in more than 25 years, shows how neglected this disease, and its survivors, are.
Where do you find noma?
Noma is most prevalent in low-income settings in Africa and Asia. Noma used to occur widely in Europe but disappeared as living conditions and access to healthcare improved.
The disease was first reported by Hippocrates in the the fifth century BC. The first medical description of noma was in 1595, when it was called ‘water cancer’. In Europe, cases were also reported in concentration camps during World War II.
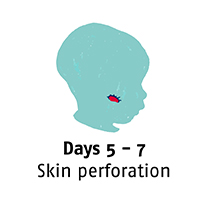
What are the symptoms?
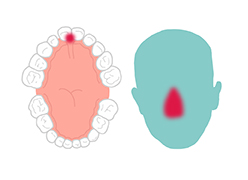
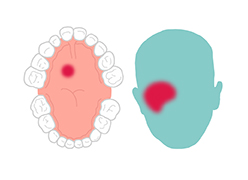
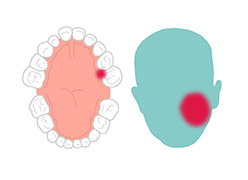
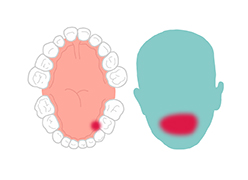
Noma starts with gingivitis, an inflammation and bleeding of the gums. In three or four days, an ulcer appears and the gums and cheek begin to swell. Before a week has passed the disease has eaten away cheek tissue and a hole appears. In the following days, the infection spreads and gangrene covers the affected area. Depending on where the infection has started, it quickly destroys the jaw, lips, cheeks, nose or eyes.


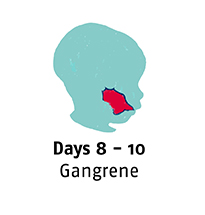
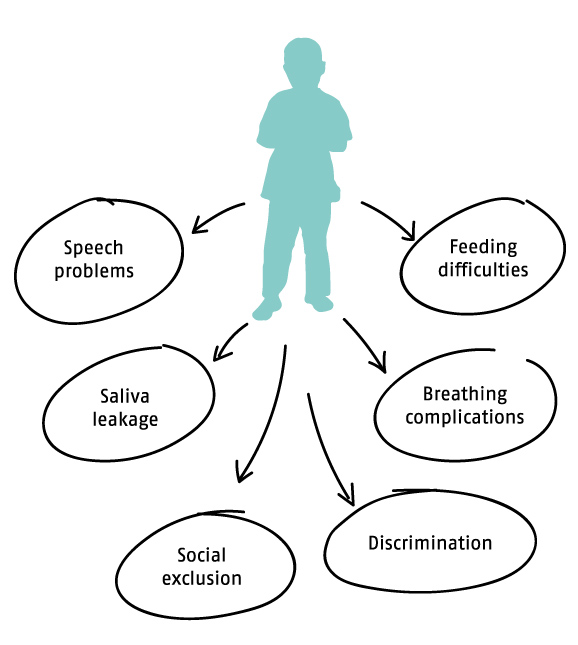
What are the consequences?
Many people who survive noma are at great risk of dying from secondary complications. They experience physical and mental consequences which isolate them from their communities and can cause mental health problems. Many people also have difficulty speaking and eating and face stigma and discrimination in their communities because of their facial disfigurement. Children can experience developmental delays because of their social isolation, or from the impact of childhood diseases linked to noma, such as measles and malaria.
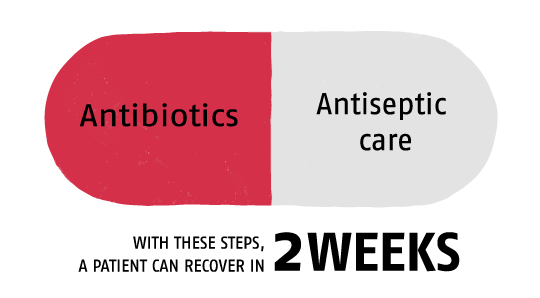
Is Noma preventable and treatable?
Noma is absolutely preventable, but only if there is knowledge about the disease and how to treat it. Good nutrition, oral hygiene and access to healthcare and vaccinations against childhood diseases all help to prevent noma.
Noma is treatable if detected and managed during the first weeks of the disease. With basic oral hygiene, antibiotics and wound dressing a patient can recover from noma within a few weeks. This is helped by managing underlying risk factors, such as malnutrition and other diseases like measles.
If it is easily treatable, why do people die from noma?
People die from this easily preventable and treatable disease because of the lack of knowledge surrounding noma. Early detection is low and once noma attacks, many families don’t have access to or can’t afford the antibiotics to treat it. Most of the people with noma live in poor and isolated areas, where access to health and dental care is almost non-existent.
Little is known about noma. It develops quickly, so the parents of a child with noma usually don't know how to identify the disease. They seek help in their community or from traditional healers, losing precious time and the opportunity to properly treat the infection.

Sufyanu, aged three, returned to his home in northern Nigeria with his parents and siblings after being treated in Sokoto Noma Hospital. He has to wait until he is older before he can have reconstructive surgery. This is because the wounds are complex and continue to change during a child’s growth.

Sufyanu, aged three, returned to his home in northern Nigeria with his parents and siblings after being treated in Sokoto Noma Hospital. He has to wait until he is older before he can have reconstructive surgery. This is because the wounds are complex and continue to change during a child’s growth.
Sufyanu, before and after noma
Sufyanu is three years old and lives in a village in Sokoto state, Nigeria. When he first arrived at Sokoto Noma Hospital, he was already acutely sick and his face was disfigured. He was also malnourished, one of the major factors that leads to noma.
Sufyanu was treated in the nutritional unit: he was given antibiotics and his wounds were cleaned and dressed. When he regained strength, he was discharged and went back home. Sufyanu will have to wait until he is older before he can have reconstructive surgery on his face. This is because the effects of the disease and the scarring changes as children grow.
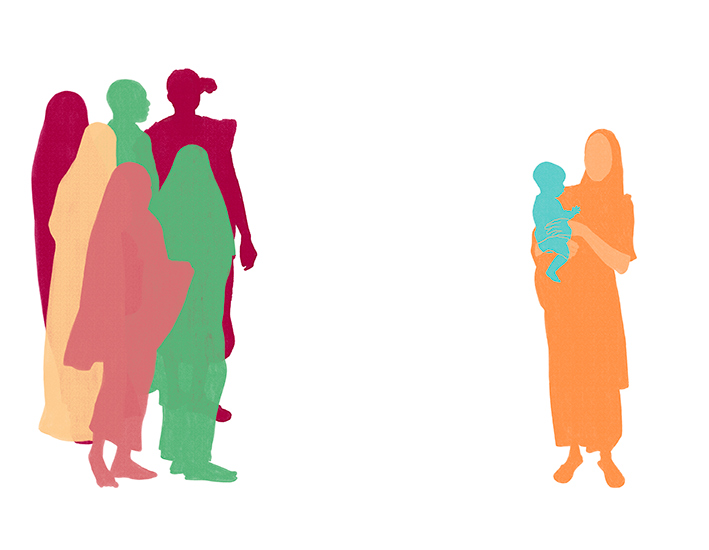
Patient journey: from infection to treatment
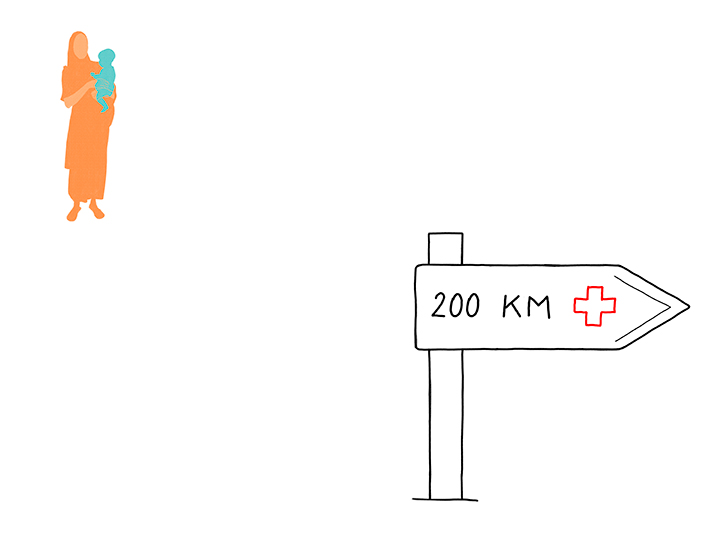
Living in isolated and extremely poor places, noma patients are difficult to find. For some, reaching a clinic or hospital is almost impossible – they may be located hundreds of kilometres away. Even when people can more easily access local clinics, often they don’t have the money to pay for medical care.
Timeline
July 25
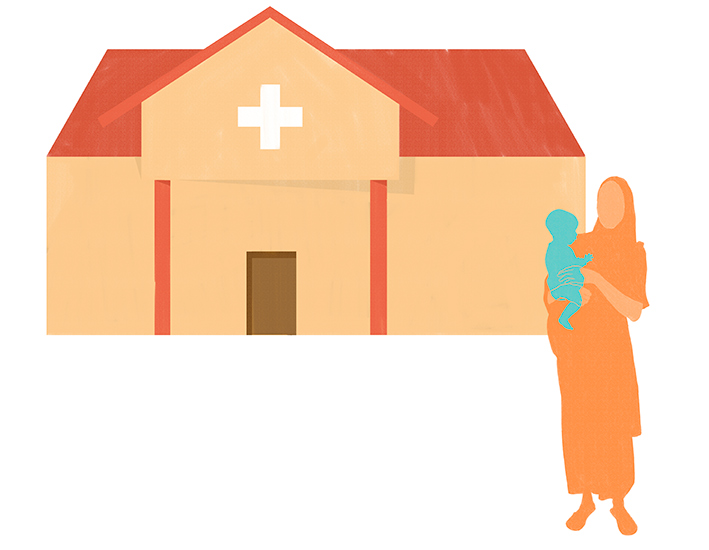
4. Reaching the nearest clinic
The mother goes to the nearest clinic which is several kilometres from their isolated village; it takes several days to reach. When they arrive, they can face two new obstacles: the lack of knowledge about noma and the cost of treatment. If they can pay for the antibiotics, the child will recover. If not, the mother has to go back home empty-handed and, usually, in a few days her child will die.July 25
5. Arrival at the hospital
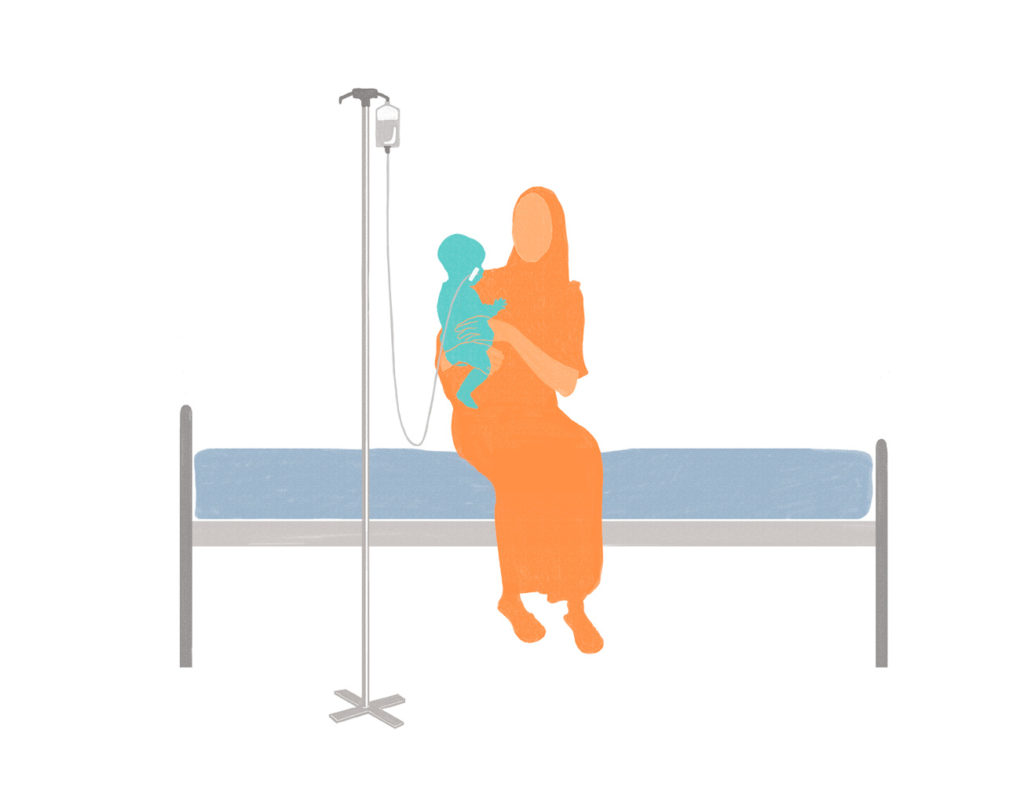
Once admitted to the hospital, the child will receive antibiotics and nutritional treatment to stabilise her/his condition and recover some of her/his strength. The child’s wounds will be dressed and the doctors will check if s/he is a candidate for reconstructive surgery. Because the wounds are complex and change over time, small children have to wait until they are older before they can have surgery.August 30
6. Starting treatment
Once admitted to the hospital, the child will receive antibiotics and nutritional treatment to stabilise her/his condition and recover some of her/his strength. The child’s wounds will be dressed and the doctors will check if s/he is a candidate for reconstructive surgery. Because the wounds are complex and change over time, small children have to wait until they are older before they can have surgery.Mohammed, when the treatment is too far away
Grema lives with his family in a city in Yobe state, Nigeria. When his young son Mohammed got sick, they didn’t know that it was noma and they didn’t know where to find help. Finally, someone told them about a hospital in Sokoto town where patients can receive free medical treatment for noma. They arrived after a two-day trip but it was too late. Little Mohammed’s face was already disfigured and in a worrying condition, because of malnutrition.
Footnotes: Drawings & infographics by Chloé Fournier / Pictures & Videos by Claire Jeantet & Fabrice Caterini © Inediz - All rights reserved